Thyroid Ultrasound
Do’s, Don’ts, and What to do with All Those Incidental Nodules!
Case: a 50-year-old female presents with a palpable lump in her neck.
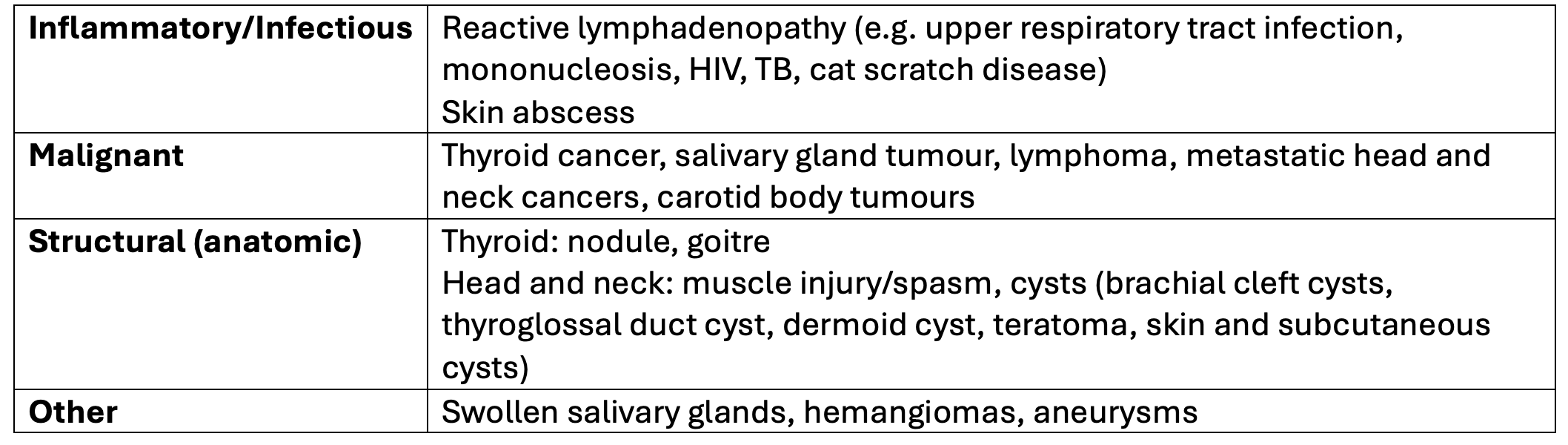
What is your differential for a neck lump/mass?
I like to use a combination of the mechanisms framework and anatomic framework to guide my diagnostic approach.
*List not exhaustive. (1)
When assessing a neck mass, its location and characteristics offer important diagnostic clues.
Midline masses are often congenital, such as thyroglossal duct cysts, but can also represent thyroid pathology or laryngoceles.
Lateral neck masses may be congenital (e.g., branchial cleft cysts) or acquired, with squamous cell carcinoma being a common malignant cause.
A pulsatile mass should raise suspicion for vascular pathology, such as a carotid body tumor overlying the carotids.
For lymphadenopathy, always consider the clinical context:
Acute cervical lymphadenopathy is most often reactive, related to viral or bacterial infections.
Sub-acute or chronic lymphadenopathy, especially in the supraclavicular region, is more worrisome and should prompt evaluation for possible malignancy.
Here is a visual representation to cue your memory for certain differential diagnoses based on anatomy:
BOTTOM LINE: You can think of inflammatory/infectious, malignant, and anatomic causes of a neck mass to guide the diagnostic process.
History & Physical Exam Tips
I like to consider 5 important aspects of the history and physical exam to help with diagnosis:
Age: most neck masses are benign in children, while in adults, the likelihood of cancer increases - especially with a history of alcohol or tobacco use and other risk factors (2).
Location: the location of the lump provides clues about its cause. E.g. midline masses are more likely to be thyroglossal duct or dermoid cysts, while lateral masses may be related to lymph nodes, salivary glands, or brachial cleft cysts (2). A mass on the thyroid gland could be a thyroid nodule (benign or malignant).
Duration: an acute lump is more likely to be inflammatory/infectious, while a lump present for weeks to months may be malignant or congenital (e.g. brachial cleft cysts, dermoid cysts).
Systemic symptoms: pain, tenderness, redness, warmth, and associated symptoms like fever, and sore throat may point to in inflammatory/infectious cause. Dysphonia/hoarseness, dysphagia, odynophagia, referred otalgia, weight loss, anorexia, malaise, and unintentional weight loss may point to more sinister causes like a head and neck malignancy (1,2).
Risk factors: e.g. exposure to ionizing radiation, family history of thyroid cancer or cancer syndromes should be assessed.
Consistency: soft, mobile masses are more likely to be benign; hard, fixed, or painless lumps are more concerning for malignancy (1,2).
🚩 Red flags for head & neck cancers: older age, smoking history, head/neck radiation, unintentional weight loss, drenching night sweats, hoarseness/vocal changes, neck tightness, dysphagia, persistent lymphadenopathy NYD (>4-6 weeks).
BOTTOM LINE: consider age, location, duration, systemic symptoms, risk factors, and consistency of the lump to differentiate between benign and sinister causes.
Back to the case: the lump is palpated over the thyroid gland, it is hard, mobile, and painless. It has been there for a month. She has no concerning systemic symptoms, and no past medical history. She has no specific risk factors for thyroid cancer, she does not smoke or drink alcohol. She has no signs or symptoms of thyroid dysfunction. What next?
Diagnostic Imaging: Thyroid
What is the first line imaging modality for suspected thyroid gland abnormalities? Thyroid ultrasound (3). It is a non-invasive, radiation-free method that effectively visualizes the thyroid and surrounding tissues. It can identify nodules and assess their characteristics (solid vs. fluid-filled), and guide fine-needle aspiration (3).
What are some other imaging options?
Radioiodine thyroid scans: this nuclear medicine test is often used to evaluate suspected thyrotoxicosis (e.g. from hyperthyroidism), may be used to differentiate between benign and cancerous thyroid nodules, staging thyroid cancer, and monitoring thyroid cancer treatment (4). This scan can detect areas of the thyroid that are overactive (producing too much thyroid hormone) vs. under-active (producing too little thyroid hormone).
CT: thyroid disorders tend to have non-specific CT appearances, and incidental findings are common on neck CT. Incidental finding management depends on the nodule size, age of the patient, and clinical correlation (e.g. health status, lymphadenopathy) (5). CT can play a role in preoperative planning in patients with large symptomatic goiter (5). Incidental thyroid nodules are detected on about 16% of head and neck CTs, which can lead to more testing (e.g. thyroid ultrasound) (6).
When to order a thyroid ultrasound:
If there is a palpable nodule, lumpy thyroid gland, or enlarged thyroid gland (with or without abnormal thyroid function tests) (7). Note: The vast majority of patients with thyroid malignancy have normal thyroid function tests (8).
If there is an incidental finding of thyroid abnormality (e.g. nodule) and the radiologist recommends further testing/imaging/monitoring.
When NOT to order a thyroid ultrasound:
Do not order a thyroid ultrasound in patients with abnormal thyroid function tests unless there is a palpable abnormality of the thyroid gland (e.g. palpable nodule, lumpy thyroid, enlarged gland) (7).
Do not order screening thyroid ultrasounds - this results in over diagnosis and over treatment without improving patient outcomes (6).
If a patient is presenting with dysphagia - it could be for a multitude of reasons. Don’t jump to ordering a thyroid ultrasound, and instead follow a careful diagnostic approach to dysphagia.
Rationale:
Incidental thyroid nodules are common, are often unrelated to abnormal thyroid function tests, and may divert clinical evaluation to assess the nodules, rather than thyroid dysfunction. Incidental findings (thyroid nodules) can lead to unnecessary testing, such as fine needle aspiration (7).
Thyroid nodules are detected by ultrasound in up to 68% of healthy patients, and most thyroid nodules are detected incidentally (6).
Most thyroid nodules are benign (90-96%). Thyroid cancer is a relatively uncommon malignancy (constituting about 0.5% of all malignancies) (8). Risk factors for thyroid cancer include ionizing radiation (e.g. from cancer treatment, occupational exposure), rapid nodule growth, hoarseness, and a family history of thyroid cancer or cancer syndromes (e.g. multiple endocrine neoplasia type 2, familial adenomatous polyposis) (6). Correlate findings clinically.
BOTTOM LINE: Thyroid ultrasound is the first-line imaging test for suspected thyroid abnormalities (e.g., palpable nodule, goiter). It should only be ordered when there are concerning features on history or palpable findings on physical exam. Incidental findings may warrant further testing.
Back to the case: given the palpable thyroid abnormality, a thyroid ultrasound is ordered.
FINDINGS:
Right thyroid lobe measures: 5.0 x 1.7 x 1.4 cm
Left thyroid lobe measures: 4.8 x 1.3 x 1.7 cm
Thyroid isthmus thickness measures 0.2 cm
NODULE 1:
Location: left upper lobe
Size: 2.1 x 1.2 x 0.6 cm
Composition: solid (2)
Echogenicity: isoechoic (1)
Shape: wider-than-tall (0)
Margin: smooth (0)
Echogenic foci: none (0)
IMPRESSION:
Left upper lobe nodule measures 2.1 cm. TI-RADS 3 - mildly suspicious. FNA if >2.5cm. Follow if >1.5cm.
Thyroid Ultrasound: Interpretation Tips
As I mentioned, thyroid nodules are a very common finding, and it can be tough to interpret the results and determine next steps.
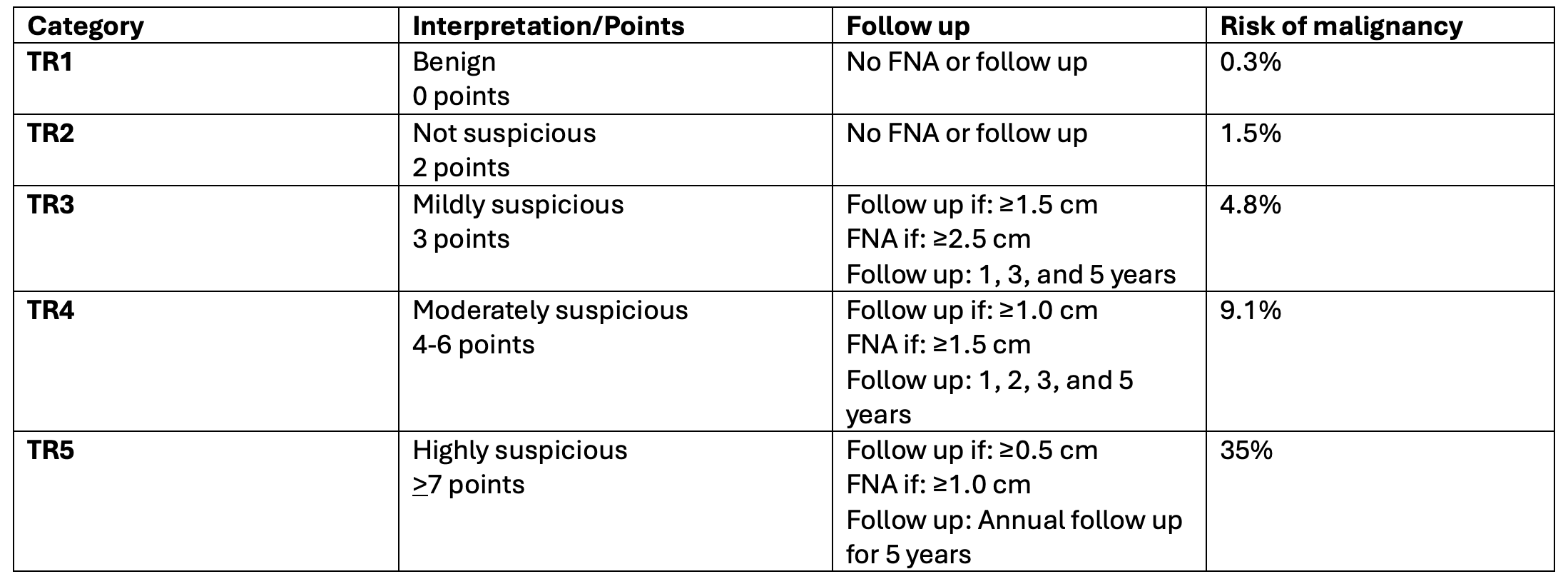
ACR TI-RADS (Thyroid Imaging Reporting and Data System) is a standardized scoring system from the American College of Radiology (2017) that helps determine which thyroid nodules on ultrasound need biopsy (FNA), follow-up, or no action (9).
The ACR system is commonly used because it detects most cancers (high sensitivity ranging from 75-97%), but it can also lead to some unnecessary biopsies since its accuracy at ruling out benign nodules (specificity) is more limited (53-67%) (10). There s also good inter-observer agreement regarding decision to biopsy (10).
How it Works
Each thyroid nodule is scored across 5 ultrasound features (10).
Composition (cystic, spongiform, mixed, solid)
Echogenicity (how bright/dark it looks)
Shape (wider-than-tall vs taller-than-wide)
Margins (smooth vs irregular, extra-thyroidal extension)
Echogenic foci (calcifications or none)
Points are added up → the total = TI-RADS category (TR1–TR5).
Higher score = higher suspicion for malignancy.
Note: Predominantly cystic or spongiform nodules are inherently benign; if these features are present they are automatically TR1 (10).
TI-RADS Categories & Management of Thyroid Nodules
(10).
BOTTOM LINE: ACR TI-RADS detects most thyroid cancers, but can also lead to unnecessary biopsies and further testing —and once you start ultra-sounding, you may be committing your patient to years of follow-up. Before ordering, ask yourself: Will this ultrasound meaningfully change the likelihood of thyroid cancer or another significant abnormality?
Back to the case: TR3 - mildly suspicious, follow up indicated (it is >1.5cm), will repeat thyroid ultrasound in 1 year. No FNA indicated.
Join NP Reasoning Masterclass for a practical, curated educational experience for the busy NP.
References Differential diagnosis of a neck mass. In: UpToDate, Emerick, K. (Ed), UpToDate, Deschler, D.G., Hussain, Z. [Accessed 2025 Aug 19]. Available from: https://www.uptodate.com/contents/differential-diagnosis-of-a-neck-massSimo R, Leslie A. Differential diagnosis and management of neck lumps. Surgery (Oxford). 2006 Sep 1;24(9):312-22.Wong KT, Ahuja AT. Ultrasound of thyroid cancer. Cancer Imaging. 2005 Dec 9;5(1):157-66. doi: 10.1102/1470-7330.2005.0110. PMID: 16361145; PMCID: PMC1665239.Canadian Association of Radiologists. Canada. 2025 [2025; August 19, 2025]. Available from: https://car.ca/wp-content/uploads/Head-and-neck.pdfBin Saeedan M, Aljohani IM, Khushaim AO, Bukhari SQ, Elnaas ST. Thyroid computed tomography imaging: pictorial review of variable pathologies. Insights Imaging. 2016 Aug;7(4):601-17. doi: 10.1007/s13244-016-0506-5. Epub 2016 Jun 7. PMID: 27271508; PMCID: PMC4956631.Kant R, Davis A, Verma V. Thyroid Nodules: Advances in Evaluation and Management. Am Fam Physician. 2020 Sep 1;102(5):298-304. PMID: 32866364.Choosing Wisely. Endocrinology and Metabolism. [2020; August 19, 2025]. Available from: https://choosingwiselycanada.org/recommendation/endocrinology-and-metabolism/Wong KT, Ahuja AT. Ultrasound of thyroid cancer. Cancer Imaging. 2005 Dec 9;5(1):157-66. doi: 10.1102/1470-7330.2005.0110. PMID: 16361145; PMCID: PMC1665239.Tessler F, Middleton W, Grant E et al. ACR Thyroid Imaging, Reporting and Data System (TI-RADS): White Paper of the ACR TI-RADS Committee. J Am Coll Radiol. 2017;14(5):587-95. doi:10.1016/j.jacr.2017.01.046 - PubmedRadiopedia. ACR thyroid imaging reporting data system (ACR-TI-RADS). 2025. [August 19, 2025]. Available from: https://radiopaedia.org/articles/acr-thyroid-imaging-reporting-and-data-system-acr-ti-rads