Iron Deficiency Anemia: Lab Test Interpretation
If you haven’t done so already, read my blog post on understanding lab reference ranges to provide context for variation of lab reference ranges we see in practice.
Questions to always ask yourself when ordering a lab test:
Will this change my management? (i.e. have I already reached the treatment threshold? Will this test change my plan?)
Will this lab test help me rule in, or rule out, a specific diagnosis?
Refresh yourself on pre-test probability, sensitivity and specificity, and negative and positive predictive values if you haven’t in a while. These are important diagnostic test principles that help inform diagnostic testing in practice. Now - let’s get into iron deficiency anemia.
Case: You’re seeing a 46-year-old female for routine cervical cancer screening, when she tells you she has had heavy menses the last 6 months which is unusual for her. She is experiencing shortness of breath on exertion, dizziness with positional changes, and fatigue. She denies any abdominal or pelvic pain, and there is no blood in her stools. There is mild tachycardia on exam, but stable vitals otherwise. Skin, head and neck, cardiac, respiratory, abdominal, and gynecologic exams are unremarkable.
As part of your initial work up you order a complete blood count (CBC) to screen for anemia.
The CBC is ordered for a multitude of reasons – e.g. patients presenting with fatigue, weakness, weight loss, infection (the list goes on!) A common CBC pattern we detect in primary care is iron deficiency anemia (IDA).
What is iron deficiency anemia?
Iron deficiency anemia is the most common nutritional deficiency in the world, with 30% of the population being affected (1). The most common causes of IDA are gastrointestinal bleeding, and menstruation in women (2).
How do we detect IDA with a CBC? The two biggest clues are low hemoglobin and low ferritin.
What are normal hemoglobin and ferritin levels? Normal range varies depending on where you practice and the reporting lab parameters. Generally speaking:
Adult male normal hemoglobin values: 135-170 (14 to 17.5 g/dL)
Adult female normal hemoglobin values: 120-160 (12.3 to 15.3 g/dL)
Normal ferritin levels: The exact value is not well established; some clinicians may use a lower value for diagnosing iron deficiency. Generally speaking, levels of <30 or <40 are considered low and can be used to confirm IDA (1).
In pregnancy: commonly defined as a hemoglobin of <110 g/L (<11 g/dl), with some suggesting hemoglobin <105 g/L (10.5 g/dl) (3).
In postpartum: diagnosed at hemoglobin levels of <100g/L (<10 g/dl) (3).
What if the hemoglobin is low but ferritin is elevated? Consider the possibility of an inflammatory process. Ferritin can be falsely elevated during acute or chronic infection or inflammation. In this case, ordering fasting iron studies can be helpful to confirm the diagnosis of IDA, especially total iron binding capacity and transferrin saturation (TSAT) (3). If the TSAT is <20%, this confirms IDA, if it is >20% IDA is less likely (4).
Tip: Avoid routinely ordering an iron profile (TIBC, TSAT, iron) to diagnose iron deficiency. Low ferritin alone confirms IDA, as it is the most sensitive and specific marker of iron stores (5). Iron profiles are only useful in patients with comorbidities (e.g., infection, autoimmune disease, kidney disease, cancer), where ferritin may be falsely elevated (5).
BOTTOM LINE: IDA is diagnosed with low hemoglobin and low ferritin. If you suspect ferritin is falsely elevated, a fasting TSAT level of <20% is useful to diagnose IDA.
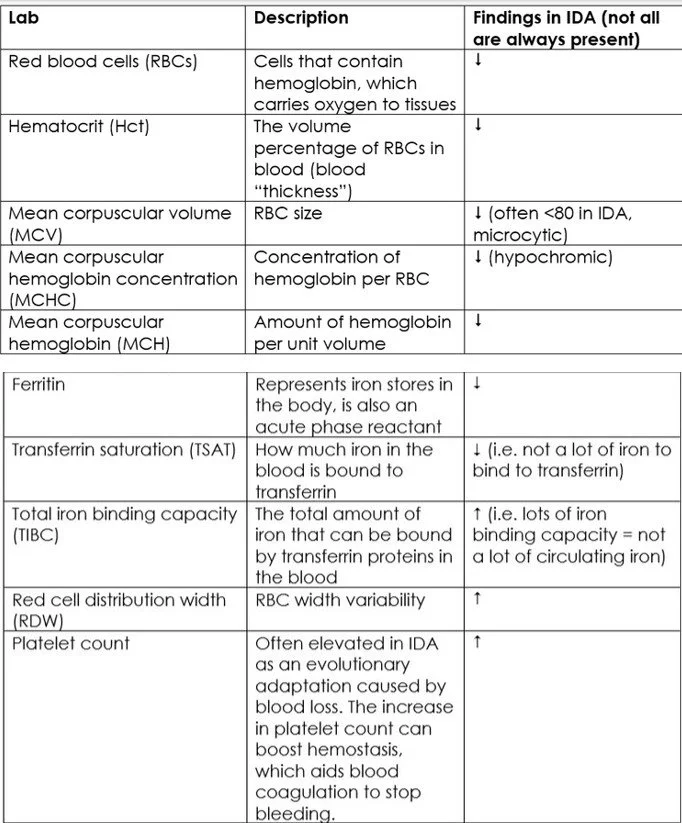
Other Lab Clues for IDA
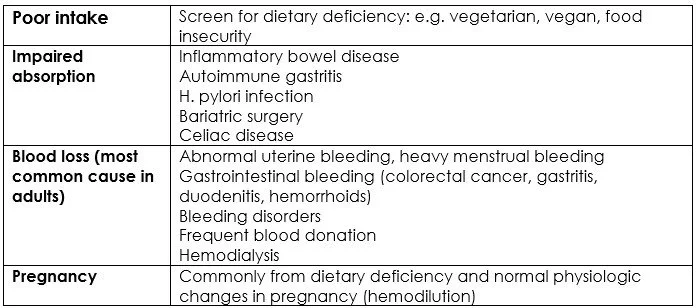
Once we identify IDA, what’s next? In all patients, the cause of iron deficiency must be identified and addressed. This is especially true for males and non-menstruating females, in whom new onset iron deficiency is strongly suggestive of blood loss from an occult gastrointestinal malignancy or other bleeding source (3). Perform a full history and physical examination to tailor your next steps and investigations.
Signs and Symptoms of IDA
(6)
Differential Diagnosis for IDA
(6)
Back to the case: You receive the CBC results. Hemoglobin is 95 g/L (9.5 g/dL). Four months ago it was 135 g/L (13.5 g/dL), hematocrit is 0.28 (low), red blood cells are 3.4 (low), platelets are 470 (elevated), ferritin is 4.
Final verdict: diagnosis is IDA, and you strongly suspect an underlying gynecologic cause. Further work up for abnormal uterine bleeding is warranted, along with treating with oral iron.
BOTTOM LINE: Once you diagnose IDA, always assess for an underlying cause. If there is no obvious cause, be suspicious for GI malignancy in adults.
ReferencesWorld Health Organisation. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Vitamin and Mineral Nutrition Information System 2011 https://www.who.int/vmnis/indicators/haemoglobin.pd
Shokrgozar N, Golafshan HA. Molecular perspective of iron uptake, related diseases, and treatments. Blood Res 2019;54:10–16.doi:10.5045/br.2019.54.1.10pmid:http://www.ncbi.nlm.nih.gov/pubmed/30956958
A. Kinga Malinowski and Ally Murji. Iron deficiency and iron deficiency anemia in pregnancy. CMAJ July 26, 2021 193 (29) E1137-E1138; DOI: https://doi.org/10.1503/cmaj.210007
Kumar A, Sharma E, Marley A, et al. Iron deficiency anaemia: pathophysiology, assessment, practical management. BMJ Open Gastroenterology 2022;9:e000759. doi: 10.1136/bmjgast-2021-000759
Choosing Wisely. 2024. Clinical biochemistry. Available from https://choosingwiselycanada.org/recommendation/clinical-biochemistry/
Auerbach, M. DeLoughery TG. 2025. Diagnosis of iron deficiency anemia in adults. Up To Date.