Syphilis Lab Test Interpretation
🔎 Case: You ordered syphilis serology in an asymptomatic patient requesting routine STI testing. HIV, trichomoniasis, chlamydia, and gonorrhea testing all return negative. Syphilis serology returns positive:
Non-treponemal test: RPR 1:16
Confirmatory treponemal test: TPPA reactive
There are no prior syphilis labs on file, and no known prior infection.
What are your next steps?
Syphilis: An Overview
What is syphilis?
A systemic infection caused by the spirochete Treponema pallidum (1).
Rising prevalence: Global syphilis rates have steadily increased since 2012, including congenital syphilis (2). Syphilis is now the second most common infectious cause of stillbirth worldwide, and current congenital syphilis rates are the highest in over 30 years (2).
Pregnancy considerations: Maternal–fetal transmission can occur at any stage, with serious fetal outcomes in the second and third trimesters, including: early fetal death, stillbirth, neonatal death, preterm birth, low birth weight, and congenital infection (1).
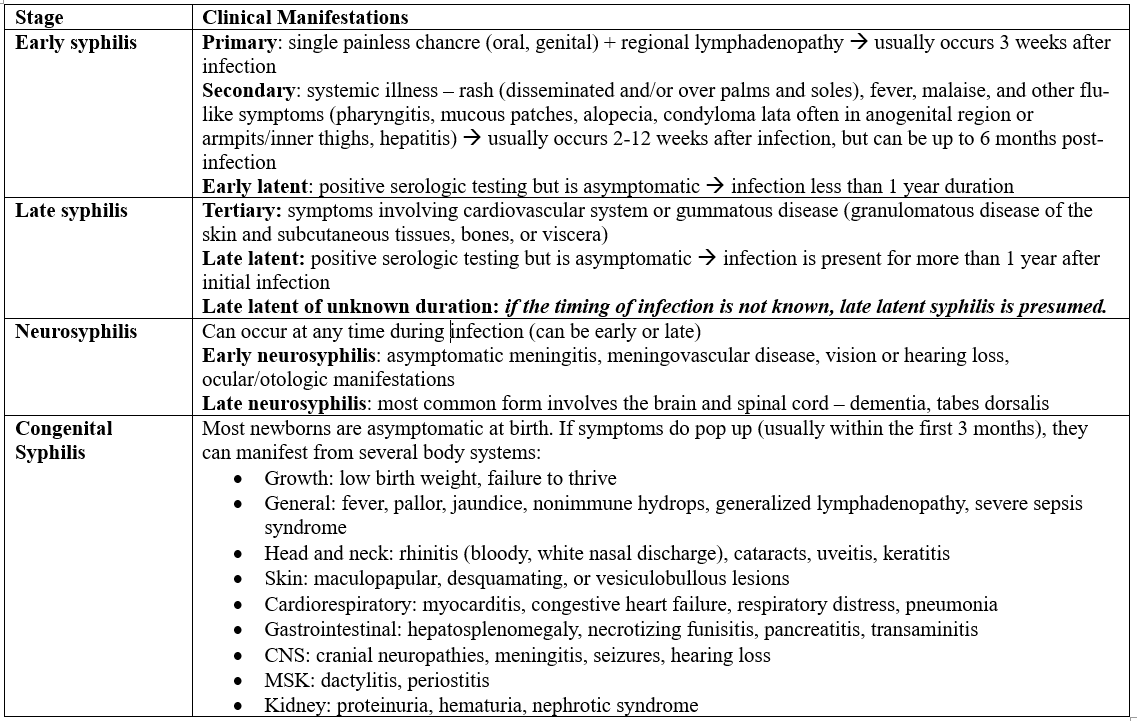
Clinical features: Symptoms mirror those in non-pregnant patients and vary by stage. Remember: syphilis is a reportable disease (1,3). As we recall, there are different stages of syphilis infection summarized in the table below:
Ordering & Interpreting Syphilis Testing: A Practical Guide
Testing in Adults
1. Non-treponemal tests (RPR, VDRL)
First-line screening
Quantitative (titers, e.g., 1:8)
Titers decline with effective treatment, which is used to monitor response
2. Treponemal tests (TPPA, FTA-ABS)
Confirm a positive non-treponemal result
Qualitative; detect antibodies specific to T. pallidum
Remain positive for life in many patients, however treponemal seroreversion reported in up to 24% of early-treated patients (i.e. subsequent negative testing)
Pearl: Early infection can yield false-negative results if antibodies have not yet formed
Screening & Testing in Pregnancy
Universal screening at first prenatal visit. Repeat at 28–32 weeks and at delivery for high-risk individuals (4,5).
High-risk factors may include:
Substance use
Concurrent STIs
New or multiple sexual partners
Partner with STI
Transactional sex
Late or absent prenatal care
Incarceration (patient or partner)
Unstable housing or homelessness
Important nuance: Biologic false-positive non-treponemal and treponemal tests are relatively common in pregnancy, reinforcing the need for confirmatory testing (4,5).
Interpreting Results
Reactive non-treponemal test (RPR/VDRL) → confirm with treponemal test (TPPA/FTA-ABS)
If confirmatory testing is negative:
Could represent very early infection or a false positive
Repeat treponemal testing in 2–4 weeks
When in doubt: consult infectious disease!
Testing in the Newborn
Do not use treponemal tests (maternal antibodies cross the placenta)
Use non-treponemal tests (RPR/VDRL)
Diagnosis is confirmed if infant titers are four-fold higher than maternal titers at delivery
Lower titers may still indicate congenital syphilis if RPR is positive and physical findings are abnormal (6,7)
Clinical pearls:
Always test for HIV (frequent co-infection)
Lab clues for congenital syphilis may include anemia, thrombocytopenia, leukocytosis, elevated CRP, and transaminitis (6,7)
🧪 For weekly lab test interpretation pearls, case-based breakdowns, practical prescribing tips, and practice-changing insights, join NP Reasoning Masterclass.
Treating Syphilis
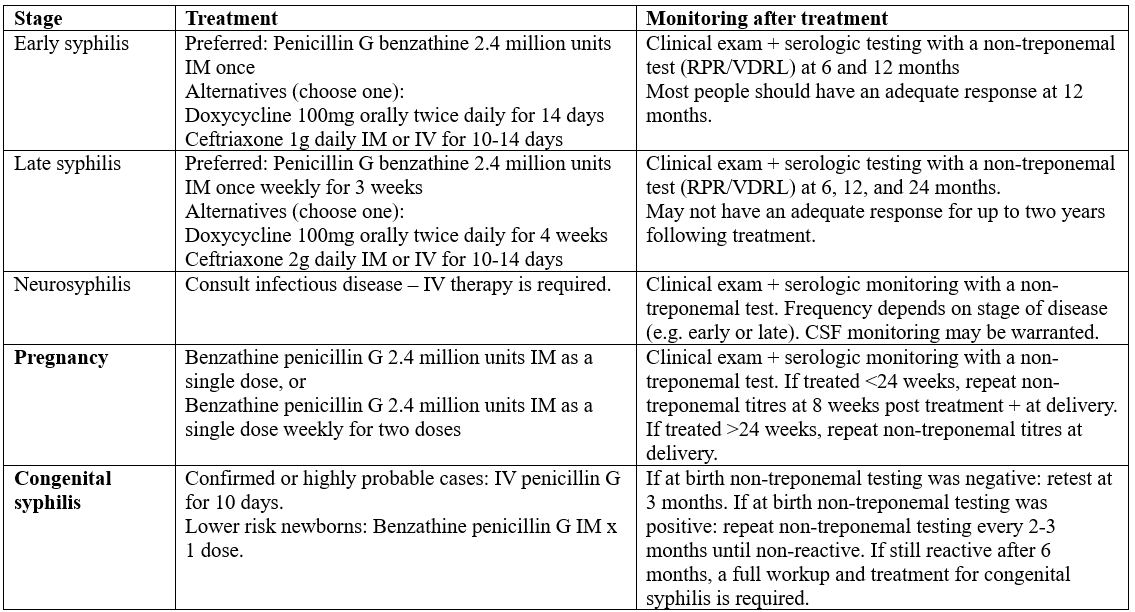
Adults: Treatment depends on suspected stage.
Non-pregnant adults: Penicillin, doxycycline, or ceftriaxone
Pregnant adults:
Penicillin is the only recommended therapy
IgE-mediated penicillin allergy → consider referral for allergy assessment +/- desensitization
No satisfactory alternatives exist (8)
Congenital Syphilis:
Confirmed/highly probable cases: IV penicillin G ×10 days
Lower-risk newborns: Single IM dose of benzathine penicillin G
No treatment required only if mother was adequately treated before pregnancy and titers remained low and stable throughout gestation
Prognosis is excellent when treated within the first 3 months of life (7)
A Note on the Jarisch–Herxheimer Reaction
This is an ccute, self-limited febrile reaction within 24 hours of treatment
Occurs in 10–35% of cases, most commonly early syphilis (5)
Symptoms: fever, headache, myalgias, rigors, hypotension, worsening rash, rarely neurologic or obstetric complications
Management: cannot be prevented, but NSAIDs or antipyretics reduce severity; usually resolves in 12–24 hours
Monitoring Treatment Response
Treatment success: Four-fold decline in non-treponemal titers (e.g., 1:32 → 1:8). In pregnancy, titers may not drop significantly before delivery (8).
Treatment failure or reinfection:
Less than four-fold decline
Four-fold increase strongly suggests reinfection or failure (8)
Seroreversion: Loss of non-treponemal antibodies after successful treatment
Common in early syphilis; less predictable in late disease
Treponemal seroreversion reported in up to 24% of early-treated patients
Monitoring frequency: Depends on stage, baseline titers, prior infection, future exposures, and HIV status (8).
*Note: Patients with HIV are typically monitored more frequently.
Common Clinical Scenarios
Scenario 1: If you have a prior non-treponemal test (RPR/VDRL) on file with a low titre e.g. 1:4, and upon re-testing titres are higher (e.g. 1:16) - this strongly suggests re-infection (or treatment failure) with a 4-fold increase in titres.
Scenario 2: If you have a prior non-treponemal test (RPR/VDRL) on file with a low titer (e.g. 1:4), and repeat testing six months later shows a higher titer (e.g. 1:8), this does not meet criteria for a four-fold increase. However, it should prompt clinical reassessment, including review of the patient’s prior stage of syphilis (if known), adequacy and timing of prior treatment, and ongoing risk factors for reinfection. Close follow-up with repeat serologic testing is warranted.
Scenario 3: You have an asymptomatic patient with both positive non-treponemal and treponemal tests, but no prior syphilis serology is available and the duration of infection is unclear. In this situation, syphilis should be presumed to be late latent (or latent of unknown duration) and treated accordingly – this is our patient!
Scenario 4: You have an asymptomatic patient with a current non-treponemal titer of 1:16 and prior documented serology showing an RPR of 1:4 with a positive treponemal test six months earlier. With documented infection within the past year and rising titers, this is most consistent with early latent syphilis (<1 year duration) and should be treated as such.
Top Take-Home Points:
Non-treponemal tests are ordered first (RPR/VDRL), if positive, treponemal testing (TPPA/FTA-ABS) is used to confirm infection
Syphilis lab interpretation can be tricky! A four-fold change in non-treponemal testing (RPR/VDRL) defines treatment response or reinfection.
Ambiguous case despite your expert detective work? Consult infectious disease!
References
Hicks CB, Clement M. Syphilis screening and diagnostic testing. In: UpToDate [Internet]. Waltham (MA): UpToDate; 2024. Available from: https://www.uptodate.com/contents/syphilis-screening-and-diagnostic-testing
Korenromp EL, Rowley J, Alonso M, Mello MB, Wijesooriya NS, Mahiané SG, Ishikawa N, Le LV, Newman-Owiredu M, Nagelkerke N, Newman L, Kamb M, Broutet N, Taylor MM. Global burden of maternal and congenital syphilis and associated adverse birth outcomes—estimates for 2016 and progress since 2012. PLoS One. 2019;14(2):e0211720. doi:10.1371/journal.pone.0211720. PMID: 30811406. PMCID: PMC6392238.
Government of Canada. Staging syphilis in adolescents and adults: selected physical exam findings according to stage of disease [Internet]. Ottawa (ON): Public Health Agency of Canada; 2024. Available from: https://www.canada.ca/en/public-health/services/publications/diseases-conditions/staging-syphilis-infection-adolescents-adults-selected-physical-exam-findings-stage-of-disease.html
Centers for Disease Control and Prevention, Division of STD Prevention. State statutory and regulatory language regarding prenatal syphilis screenings in the United States [Internet]. Atlanta (GA): CDC; 2025 Jun 2. Available from: (link not provided).
Norwitz ER, Hicks CB. Syphilis in pregnancy. In: UpToDate [Internet]. Waltham (MA): UpToDate; 2025. Available from: https://www.uptodate.com/contents/syphilis-in-pregnancy
Stafford IA, Workowski KA, et al. Syphilis complicating pregnancy and congenital syphilis. N Engl J Med. 2024;390(3):242–253. PMID: 38231625.
Lago EG, Vaccari A, Fiori RM. Clinical features and follow-up of congenital syphilis. Sex Transm Dis. 2013;40(2):85–94. PMID: 23324972.
Government of Canada. Syphilis guide: treatment and follow-up [Internet]. Ottawa (ON): Public Health Agency of Canada; 2024. Available from: https://www.canada.ca/en/public-health/services/infectious-diseases/sexual-health-sexually-transmitted-infections/canadian-guidelines/syphilis/treatment-follow-up.html