Diagnostic Imaging for a Breast Lump (and other breast concerns)
Case: A 50-year-old female presents with a breast concern. She believes she palpated a small lump in her left breast but is more concerned about skin thickening over the same area.
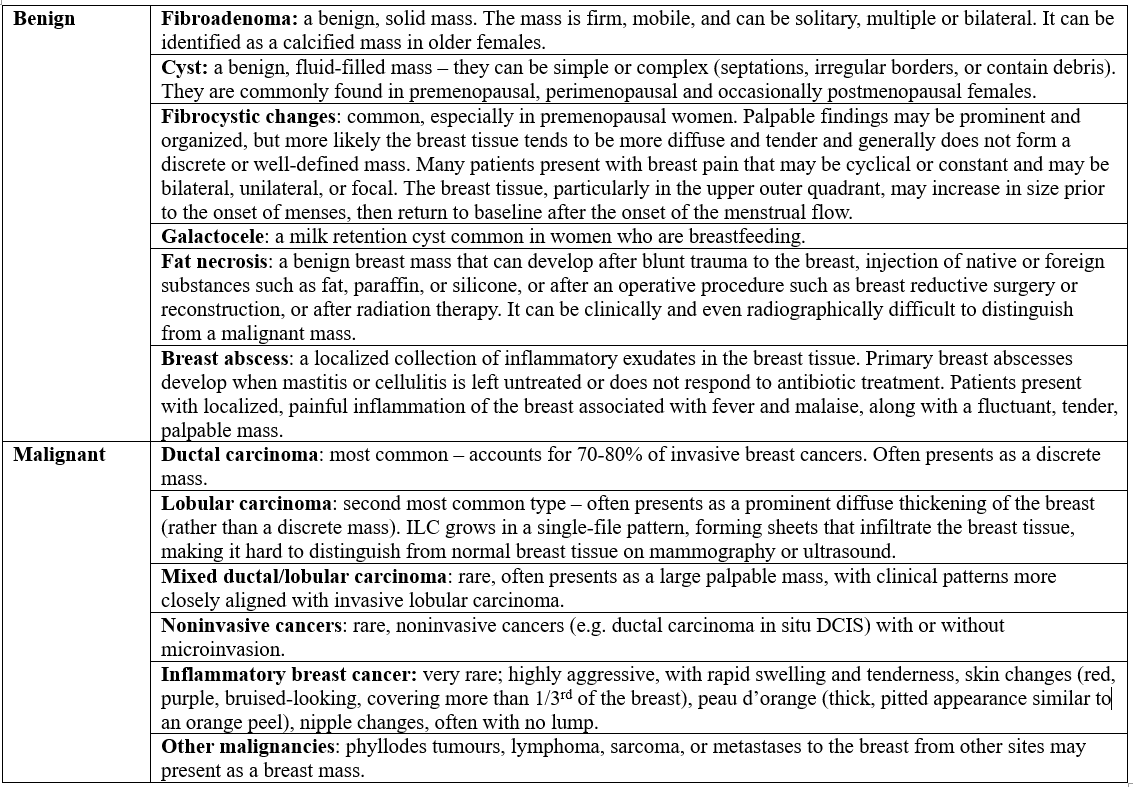
Step 1: Think Broad — Benign vs Malignant - Differential for a Breast Lump
Palpable breast lumps are common, and most are benign. Approximately 90% or more of palpable breast masses in females in their 20s–50s are benign (Elmore). However, malignancy must always be ruled out.
Patients often present after incidentally discovering a lump — but they may also present with:
Skin changes
Nipple changes
Breast asymmetry
Pain
Discharge
It’s helpful to organize your differential into benign and malignant causes.
source: (2)
Step 2: History - Adjust Your Pre-Test Probability
The goal of the history is to adjust your suspicion for malignancy.
Here are some high-yield history questions
Precise location of concern
Duration and progression of the change
Waxing/waning with menstrual cycle
Change in breast size or symmetry
Skin changes: colour changes (e.g. bruising), skin thickening, dimpling
New nipple inversion
Nipple discharge characteristics
Red Flags for Nipple Discharge
Spontaneous (without stimulation)
Unilateral
Bloody, clear, or thick
Associated with new mass
Additional considerations:
Breast pain (cyclical vs spontaneous)
Trauma (e.g. car accident), may cause a breast mass due to the development of fat necrosis or hematoma
Prior breast surgery or radiation
Risk factors (BRCA1/2, first-degree relatives, early menarche, past/current use of contraceptive pills or current use of hormone replacement therapy, alcohol: 2-5 drinks/day)
Protective factors (breastfeeding >16 months lifetime, multiparity, exercise)
(2)
Step 3: Physical Exam - Helpful, But Limited
How Good Is the Clinical Breast Exam?
Bottom line: not great.
Sensitivity is generally lower than mammography, ranging widely from 50-90%, depending on the clinician’s skill level; whereas specificity is higher, reported as 88-99% (3). Overall, not great at ruling cancer out, but decent at ruling cancer in if a palpable abnormality is found (3).
What factors increase accuracy of ruling in, or ruling out breast cancer on exam?
A thorough, unhurried exam
Training and expertise
Tumour characteristics: larger, superficial tumours are easier to detect than small or deep ones
If you want a quick re-cap on the clinical breast exam, this Stanford Medicine resource provides a good overview.
💡Clinical pearl: Invasive lobular carcinoma often does not present as a discrete mass. Skin thickening may be the only clue. Listen carefully to patients reporting texture changes.
Back to the Case:
Pertinent history clues:
Patient discovered the small lump in her left breast 1 month ago, skin thickening the last few weeks over the left breast.
She cannot palpate the small lump today.
No colour changes, nipple inversion, dimpling, or discharge.
No personal or family history of breast cancer.
On exam: no palpable lump is felt, but over the left breast, in the upper right quadrant the skin does feel a thicker texture compared with the rest of the breast. There is no palpable lymphadenopathy.
Updated differential: the palpable breast lump felt by the patient could be benign if it disappeared, or it could have been missed on exam. Although the patient doesn’t have any significant risk factors for breast cancer, the new onset skin thickening is a concerning finding. Ultimately, malignancy needs to be ruled out. But where do we go from here? An ultrasound? Mammogram? Or MRI? Let’s dive into the pearls and pitfalls of breast imaging – so that you never miss a critical diagnosis.
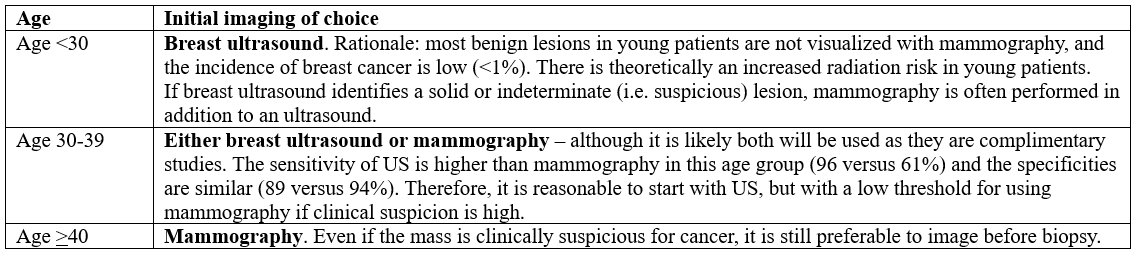
Step 4 - Diagnostic Imaging: Choosing the Right Test for a Breast Concern
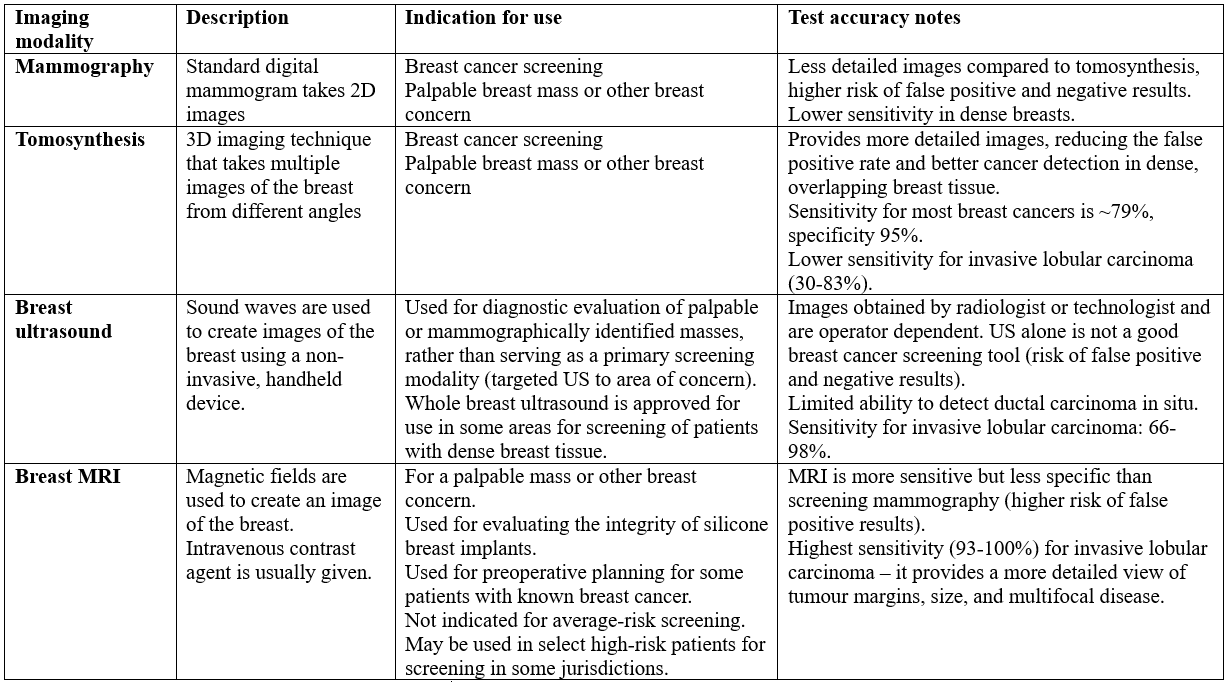
Imaging options for breast concerns include mammography (including tomosynthesis where available), targeted breast ultrasound, or an MRI (1). Approximately 85% of breast cancers are detectable with breast imaging (4). The initial diagnostic imaging tests of choice depends on the patient’s age and the degree of clinical suspicion/radiologic suspicion (4).
Initial Imaging Selection based on age (National Comprehensive Cancer Network and American College of Radiology ACR Appropriateness Criteria)
sources: 1,5,6
Now let’s review different the imaging modalities, including how they work, indications for use, and test characteristics:
sources: 4, 7, 8
Bottom line: Most guidelines use age to determine the initial imaging modality for a breast concern (remember this is different from breast screening guidelines):
<30 = US
30-39: US + mammo (usually a combo)
>40: mammo
Mammogram (especially 3D tomosynthesis) has relatively high sensitivity and specificity for most breast cancers, but can miss invasive lobular carcinoma (MR has higher accuracy for this breast cancer). Breast US is useful for imaging a targeted area of concern, to guide breast biopsies, and helps correlate mammographic findings.
Back to the case: at age 50, the initial diagnostic imaging choice would be mammography. On the test requisition you include the history including the patient reporting a palpable mass in the left breast (which you could not palpate on exam), and skin thickening over the left breast. The final interpretation of the radiology report is as follows:
BI-RADS 1: Normal or benign findings. The patient can continue with routine annual screening mammography.
Interpreting Mammogram Results
Majority of breast cancers are diagnosed with an abnormal mammography – but not all mammographic findings represent cancer. Following mammography and possibly breast ultrasound, if a mass is found it’s assigned to one of the Breast Imaging-Reporting and Data System (BI-RADS) assessment category – which guides further management:
BI-RADS 1 or 2: Normal or benign findings. The patient can continue with routine annual screening mammography.
BI-RADS 3: Probable benign findings. The patient should repeat diagnostic mammogram in six months.
BI-RADS 4: Suspicious for malignancy. BI-RADS 4 lesions have a 3 to 94 percent risk of malignancy that could be either ductal carcinoma in situ (DCIS) or invasive cancer. Management may be affected by the patient's age, comorbidities, and the type of cancer.
BI-RADS 5: Highly suggestive of malignancy. Such lesions have a ≥95 percent chance of being malignant. In addition to biopsy, BI-RADS 5 (and some BI-RADS 4C [50 to 94 percent risk of malignancy]) patients would benefit from early surgical consultation (5).
As with any diagnostic test, there is no such thing as a perfect test. This means we have to interpret results with caution, correlate results clinically, and determine if further diagnostic evaluation is needed. Since mammograms are a common initial test for breast concerns, it’s important to highlight factors that impact accuracy of mammography, so that you can incorporate these factors into result interpretation:
Factors That Affect Mammography Accuracy
Patient Factors
Younger age → lower sensitivity
Dense breasts (category B, C) → 10–29% lower sensitivity (recall: breast density is determine on imaging, not on clinical exam). Density categories:
A: Almost entirely fatty
B: Scattered fibroglandular
C: Heterogeneously dense
D: Extremely dense
Note: Dense breasts are common and not abnormal.
Tumour Factors
Lobular carcinomas are harder to detect
Rapidly growing tumours may be missed
BRCA-associated cancers may evade detection
Radiologist Factors
Experience and volume of reports read matter for more accurate interpretation
Breast imaging specialists improve accuracy
Back to the case: although reported as BIRADS-1, you are still concerned. You bring your patient back to review results and re-examine. There is persistent the skin thickening over the left breast. You are concerned the mammogram missed a possible malignancy – something like invasive lobular carcinoma. You decide to order an MRI based on your clinical suspicions, which has better sensitivity and specificity for this form of breast cancer.
Results: MR of the left breast revealed extensive cancer throughout the left breast and axillary lymph nodes. This could indicate an invasive lobular carcinoma. Next steps would be arranging an urgent breast biopsy for confirmation.
💡Clinical Pearl: the diffuse nature of invasive lobular carcinoma often leads to false reassurances from normal imaging results (mammography or breast ultrasound), as there may not be a clear lump to detect (9). If the imaging results don’t fit the clinical picture, breast symptoms aren’t resolving, and you don’t have a concrete answer for the patients signs and symptoms, it’s time to investigate further.
🧠Top Take Home Points:
Any unilateral breast changes, including skin firmness, thickness, colour changes, nipple changes, should be taken seriously – even when initial imaging appears normal.
Invasive lobular carcinoma is a unique presentation – often without a palpable mass because of its diffuse nature; when clinical suspicion is high, further evaluation with an MRI is often needed for diagnosis.
Match the imaging modality to your clinical suspicion: Mammography is first-line in women ≥40 with a breast concern, but MRI has the highest sensitivity for invasive lobular carcinoma. Escalate when the clinical picture warrants it.
👉 Sign up to Masterclass for weekly case-based breakdowns, practical prescribing tips, diagnostic test insights, and practice-changing updates, delivered straight to your inbox.
References1. Elmore JG, Barton MB, Moceri VM, Polk S, Arena PJ, Fletcher SW. Ten-year risk of false positive screening mammograms and clinical breast examinations. N Engl J Med. 1998 Apr 16;338(16):1089–1096. doi:10.1056/NEJM199804163381601.2. Sabel MS, Chagpar AB, editors. Clinical manifestations, differential diagnoses, and clinical evaluation of a palpable breast mass. In: UpToDate [Internet]. Waltham (MA): UpToDate Inc.; 2025 [cited 2026 Feb 18]. Available from: https://www.uptodate.com/contents/clinical-manifestations-differential-diagnosis-and-clinical-evaluation-of-a-palpable-breast-mass3. Fenton JJ, Rolnick SJ, Harris EL, Barton MB, Barlow WE, Reisch LM, et al. Specificity of clinical breast examination in community practice. J Gen Intern Med. 2007 Mar;22(3):332–337. doi:10.1007/s11606-006-0062-7.4. Esserman LJ, Joe BN, Chagpar AB, Hayes DF, Whitman GJ, editors. Diagnostic evaluation of suspected breast cancer. In: UpToDate [Internet]. Waltham (MA): UpToDate Inc.; 2023 [cited 2026 Feb 18]. Available from: https://www.uptodate.com/contents/diagnostic-evaluation-of-suspected-breast-cancer5. Magny SJ, Shikhman R, Keppke AL. Breast Imaging Reporting and Data System. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan– [updated 2023 Aug 28; cited 2026 Feb 18]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459169/6. Lehman CD, Lee CI, Loving VA, Portillo MS, Peacock S, DeMartini WB. Accuracy and value of breast ultrasound for primary imaging evaluation of symptomatic women 30–39 years of age. AJR Am J Roentgenol. 2012 Nov;199(5):1169–1177. doi:10.2214/AJR.12.8842.7. Nelson HD, Cantor A, Humphrey L, et al. Screening for breast cancer: a systematic review to update the 2009 U.S. Preventive Services Task Force recommendation. In: Evidence Syntheses, No. 124 [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2016 Jan [cited 2026 Feb 18]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK343820/8. National Cancer Institute. Breast cancer screening (PDQ®)–health professional version [Internet]. Bethesda (MD): National Cancer Institute; [cited 2026 Feb 18]. Available from: https://www.cancer.gov/types/breast/hp/breast-screening-pdq9. Limaiem F, et al. Lobular breast carcinoma. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan– [updated 2023 Jun 3; cited 2026 Feb 18].